
Welcome to Wound Care Today; the place for you to share your successes and concerns and learn about what is happening in wound care, globally, nationally, locally, politically and clinically.

Wound malodour is often an unpleasant side-effect experienced by patients with hard-to-heal wounds. The impact on mental and physical wellbeing is profound and can result in embarrassment, social isolation, depression and nausea. This list is not exhaustive and understanding the effect of malodour on an individual should be considered during holistic patient assessment. This article presents the findings of two surveys which aimed to gain a deeper understanding of the impact that malodour has on individuals and also the challenges experienced by healthcare professionals (HCPs) when treating patients with malodorous wounds. The patient survey was completed by 29 people, of which 76% (n=22) experienced wound malodour. The HCPs survey was completed by 789 respondents and challenges highlighted included lack of training and education, limited access to appropriate dressings and managing patient expectations.
.jpg)
Hard-to-heal wounds present a significant challenge in healthcare, requiring a comprehensive understanding of the wound healing process and effective management strategies. A survey was conducted by the Journal of Community Nursing among its registered online members to explore the current opinions and challenges faced by healthcare professionals (HCPs) who are involved in delivering wound care, including opinions on advanced wound therapies. The survey, which consisted of 14 questions, highlighted some interesting findings including several challenges experienced when treating patients with wounds. Results revealed that 69% (n=311) of participants indicated a lack of time and resources as the primary barrier. Patient compliance (67%, n=303), limited access to advanced therapies (47% n=211), insufficient training (37%), and cost pressures (32% n=145) were also significant concerns. Despite these challenges, most respondents (63%, n=281) felt ‘somewhat satisfied’ with their ability to manage wounds, but found the process frustrating due to the difficulties that they encountered.

This paper reports on the results of a clinician survey exploring the real world experience of clinicians using a range of gelling fibre dressings (Exufiber and Exufiber Ag+; Mölnlycke Healthcare, Gothenburg SW).

As a clinician, it is important that you are aware of all the latest new products that have the potential to improve outcomes for you and your patients. Each month, Wound Care Today will highlight a product that is new, improved or innovative to keep you up to date with what is available. This month, we focus on eKare inSight®, a unique and easy to use Wound Management Digital System (WMDS) that transforms a smartphone into a medical device enabling standardised, accurate wound assessment at the point of care.

Lymphoedema is a chronic, progressive condition, which can have a significant impact on patients ó both physically and psychologically. While there is no cure, it is vital that the condition is effectively managed to prevent deterioration and its impact on patient quality of life.

A specialist wound telehealth service was established to deliver equitable service with parity of access to wound care for all residents of 38 nursing homes in Sussex with wounds of any type (n=579). All patients were managed using a systematic telehealth approach that combined digital and in-patient consultations according to established protocols and care pathways. Data for a three-year period was analysed by hand to determine patient demographics, wound type and discharge outcomes for all patients with wounds. The results showed that the mean age of patients was 86 years, with the majority being female (80% healed and 66% deceased). Referral outcomes were referred onwards (n=92), healed (n=234) or deceased (n=253). The most prevalent wound type was pressure ulceration in both healed and deceased patient groups (60% and 59%, respectively), followed by lower limb wounds (20% and 26%, respectively). Mean time to healing or death were 103 days versus 86 days, respectively. The authors concluded that the collaborative use of a specialist wound telehealth service ensured that all residents received prompt, evidence-based wound care. Healing was achieved in this vulnerable patient population, despite the existence of numerous barriers to healing. Patients nearing end of life with a wound received palliative wound management. The time to healing in this group cannot be commented upon due to lack of comparative studies in this patient population.
As healthcare professionals, our purpose is to deliver treatments and interventions to patients to aid recovery and prevent deterioration in health. But what does that look like when patients do not wish to follow advice, do not want treatment or interventions, even if that means significant consequences such as loss of limbs, sepsis or death — where do we legally stand in these situations and how do we work with patients to achieve the best possible outcomes for them? Over years of clinical experience, the authors have found that working with those who self-neglect can be complex. This is due to a range of factors, such as risks to the individual and sometimes others. Other issues involved include healthcare professionals’ views and moral conflict between respecting patient autonomy and their duty of care, challenges in trying to engage patients who may not want services involved, attempting to assess and being clear on the patient’s mental capacity, working within task-orientated systems which may not always be conducive to building rapport, and working with the patient’s socio-economic factors which impact upon their health (Research in Practice, 2020).

When patients present with red lower legs, the cause is often assumed to be cellulitis or erysipelas. There are, however, several alternative conditions which mimic the clinical signs of cellulitis or erysipelas, which can lead to misdiagnosis. It is important that the cause is correctly diagnosed to prevent inappropriate prescribing of antibiotics.

Dermatological conditions are notoriously difficult to spell! Psoriasis with its silent ‘P’ and eczema without an ‘X’. But how about hidradenitis suppurativa (HS)? Hard to spell, hard to pronounce but, more importantly, really hard to be a patient with the condition.
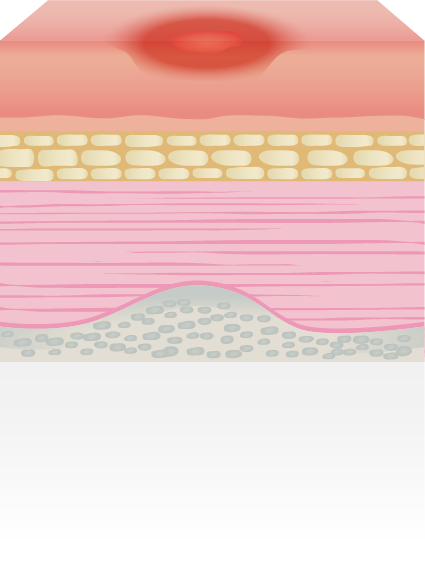
HS is a disease in which a patient develops boils and abscesses in the most intimate of areas (Figure 1); predominantly the groin and axillae.

Suboptimal management of leg ulcers has been identified as a UK-wide problem that is both costly to the NHS and a drain on nursing resources (Guest et al, 2020). The overall annual NHS cost of wound care has increased by 48% in real terms over the five years since Guest et al’s (2015) original work. Guest et al’s studies (2015; 2020) also found a common pattern with regard to a failure on the part of healthcare professionals to establish the underlying aetiology of a wound. This article highlights the importance of changing the way we treat leg ulceration in relation to identifying and managing patients with lymphovenous disease, and explores new treatments surrounding the care of leg ulceration to help break down fibrosis in complex wounds caused by lymphatic changes.

This article explores why we should adapt assessment of leg ulceration to be more mindful of the presence of lymphoedema. If clinicians can change the assessment process and begin to treat leg ucleration with a lymphatic component differently to venous oedema, this, in turn, can potentially reduce complications such as toe, foot and knee oedema. The introduction of simple changes in documentation and additional training can lead to improved outcomes for patients as well as potential cost savings for healthcare providers.

The delivery of wound care in the current climate is challenging so effective solutions are more important than ever. It is vital to be aware of the latest products and innovations that have the potential to improve outcomes.
Here, we present Mepitel® One, a gentle one-sided wound contact layer with Safetac® technology to minimise pain for patients during dressing changes.

Monika Varechova describes her experience of using medical grade honey to achieve healing of bilateral chronic VLUs in a complex patient receiving palliative care.
.jpeg)
Karen Harrison Dening, Lisa Ashworth, Annemarie Brown, Teresa Burdett and Anne Williams discuss the different ways that nurses learn and how new technologies can help to engage all learners.

With face-to-face interaction at a stand still since the beginning of the pandemic, there has been a gap in our learning where practical, interactive workshops had a huge impact. Fortunately, this October I had the opportunity to attend Wound Care Today 2021 and see the world of in-person networking reopen again.

Una Adderley discusses the importance of data collection and analysis in changing practice and outcomes.
.png)
The problem of delayed wound healing has been highlighted in several publications which has stimulated debate on variance and the need for updated care pathways. This paper demonstrates how adjunctive therapy can be added to the ‘standard care’ model, described in the National Wound Care Strategy Programme’s recommendations for lower limb wounds, to enhance outcomes for patients with ‘hard-to-heal’ lower limb wounds (NWCSP, 2020). A decision-making pathway based on published literature is described which uses wound assessment and observed response to treatment to allow the effective and targeted introduction of adjunctive therapies for ‘hard-to-heal’ wounds. This approach will allow the cost-effective introduction of new and evolving therapies, such as WoundExpressTM (Huntleigh Healthcare), which addresses the underlying problems associated with resistant lower limb oedema and compromised venous function. The pathway also indicates how other adjunctive or innovative topical wound-based treatments can be integrated to optimise outcomes while providing cost-effective care.

Cristina Quinteiro describes the use of medical grade honey to achieve healing in an elderly patient with chronic leg wounds and complex poly-morbidity.

Febe Bruwer describes the effect of using Medical Grade honey on protease levels in a variety of patients with non-healing wounds.

The delivery of wound care in the current climate is challenging so effective solutions are more important than ever. It is vital that you are aware of the latest products and innovations that have the potential to improve outcomes.
Here, we present PolyMem®, a unique multifunctional polymeric membrane dressing that is indicated for a wide range of acute, chronic and specialist painful wounds.

The delivery of wound care in the current climate is challenging so effective solutions are more important than ever. It is vital to be aware of the latest products and innovations that have the potential to improve outcomes.
Here, we present Exufiber® and Exufiber® Ag+, next generation gelling fibre dressings that use Hydrolock® Technology to optimise wound conditions so that healing can occur.

Victoria Warner, reports on the use of an Online Non-Prescription Ordering Service (ONPOS) for wound dressing procurement in an acute trust for the first time. She describes how implementing the system has resulted in many benefits including increased efficiency and formulary compliance, and a reduced number of dressings purchased and used inappropriately, resulting in significant cost savings.

Venous leg ulcers (VLUs) are known to place a significant burden on healthcare services, with unhealed ulcers costing 135% more than their healed counterparts over the course of a year (Guest et al, 2016). This is a consequence of unwarranted variation in care attributed to difficulties experienced by non-specialist clinicians caring for VLU in the community. VLU healing rates are relatively unknown, and national targets for healing do not yet exist, but there is evidence in the literature that specialist VLU services improve healing rates (Moffatt et al, 1992). Healogics is a specialist third party provider of VLU and lymphoedema services to the NHS, that takes a systematic approach to the assessment and management of these co-existing conditions. This paper presents the healing rates of 1015 people with VLU treated by Healogics for the full 65-month duration of an any qualified provider (AQP) contract. Healing rates of 86.14% were obtained in an average of 117 days in line with the published healing rates from other specialist leg ulcer services (Moffatt et al, 1992; Edwards et al, 2005). The healing rates reported in this paper demonstrate that a consistent, specialist approach to VLU management that is underpinned by best practice and national guidelines can help to achieve timely healing in the majority of patients, and can identify more complex patients for whom healing is not possible, enabling them to be placed on a maintenance pathway. The authors’ suggest that grading of VLUs according to complexity and data collection and analysis of healing rates could help to improve healing outcomes on a national level.

The Woundcare Industry Group provide further comment on the Facebook Live Question Time event that was held to facilitate discussion amongst key stakeholders about the future of wound care in England.

A Facebook Live Question Time event was held in February 2020 to facilitate discussion among stakeholders of the future of wound care services in England, which is summarised here.

The delivery of wound care in the current climate is challenging so effective solutions are more important than ever. It is vital that you are aware of the latest products and innovations that have the potential to improve outcomes.
Kliniderm® foam silicone is a gentle, conformable and comfortable dressing range, that can help to minimise pain at dressing change.

As a clinician, it is important that you are aware of the latest products and innovations that have the potential to improve outcomes for you and your patients. Each month, WCT will highlight a product that is new, improved or innovative in order to keep you up to date.

Cavity wounds can be very challenging in practice and often require adaptation of the clinical skills required for the management of most other acute and chronic wounds. Failure to manage cavity wounds effectively can result in delayed healing and an increased risk of associated complications. This in turn can place increased demands on a clinicians’ case load and increase costs for health services, as well as impacting negatively upon the patient’s quality of life. This article describes cavity wound presentation, the adaptations required in their assessment and management, and includes identifying appropriate cavity wound dressings to optimise local wound care. The importance of considering the physical and psychological wellbeing of the patient is also discussed, along with the importance of engaging them in decisions about their care and enabling self-management where appropriate.

Throughout the COVID-19 outbreak, community nursing services continue to deliver care to the vulnerable. Leg ulcer management is a significant part of this caseload. Alison Hopkins provides some practical advice on how to maximize efficiency in applying compression to this patient group, in order to reduce nurse workload and maximize outcomes for patients.

The delivery of wound care in the current climate is challenging so effective solutions are more important than ever. It is vital that you are aware of the latest products and innovations that have the potential to improve outcomes.
If you have patients on your caseload with long standing wounds, it is likely that biofilm is the cause. Here, we present AQUACEL® Ag+, an innovative dressing range that has been specifically designed to disrupt and destroy biofilm to help progress hard-to-heal wounds.

Kate Upton, registered adult nurse and fellow of the Higher Education Academy; representative for Nursing Professions on the Crisis, Disaster and Trauma Psychology Section of the British Psychological Society; independent nursing/medical tutor and medical writer; PhD student at the University of Birmingham

Alison Schofield asks if tissue viability is in crisis, and explains how WCT and TVN2Together aim to offer support.

Rachel Reece describes the development of educational resources to support 140 link workers in the efficient delivery of wound care across a large 1200 bed acute trust.

Do you find it difficult to appropriately reposition patients with complex needs using traditional pressure-relieving products? A lateral tilt pressure care mattress may be the answer to your problem. The OSKA Series5 lateral tilt pressure care mattress uses an alternating air and foam combination to provide both comfort and support to people with pressure ulcers. It is suitable as an aid in the prevention, and treatment of, pressure ulcers up to and including category 4.

Una Adderley gives an update on progress of the NWCSP to date.

Lorraine Jones describes how dressing spend was increasing year on year at the Royal Wolverhampton NHS Trust, and in order to drive efficiency, procurement of dressings was switched from supply chain to ONPOS. The process and outcomes are described.

Alison Hopkins MBE questions why, as a profession, nurses are allowing the normalisation of non-healing leg ulcers, and why proven treatments are still not being used to maximum effect.

Libby Gray asks can technology help to standardise the collection and documentation of wound measurement data?

Do you use different approaches for patients with lymphoedema and chronic oedema? If so, it may be time to rethink says Rebecca Elwell.

Kate Upton describes compassion fatigue, an increasingly reported form of stress associated with the demands of nursing in the current NHS, and questions what can be done to overcome it.

Jayne Livesey highlights the key goals and principles of delivering wound care at the end of a patient’s life.

While many general practice nurses (GPN) are already used to managing patients with multiple comorbidities, the need for complex wound care that can accompany patients with long-term conditions is on the increase, and has been for some time. So is now the time for GPNs to become experts in wound care?

Andrew Sharpe discusses three of the clinical emergencies seen in the diabetic foot — peripheral arterial disease, infection and Charcot neuro-osteoarthropathy (Charcot foot) — with the aim of enhancing knowledge and clinical skills in the management of diabetic foot disease.

We are all aware of staff shortages and the challenges they present to the NHS in all areas of practice.

At the Wound Care Today event in February 2019, three clinicians presented on the main stage for the first-time as part of an initiative offering support for first-time presenters. Here, they share their experience.

The transition from experienced nurse to tissue viability nurse specialist (TVNS) is challenging, with numerous hurdles to overcome. Here, Ali Hill reflects on her experience to date, transitioning from the management of chronic wounds in the community to specialist management of oncological wounds in a hospital setting.

Welcome to Wound Care Today; your new digital journal for all things wound care.

Welcome to Wound Care Today. I was equally surprised and proud to be asked if I would take the role of editor-in-chief for the journal.

Writing for publication is now unavoidable for healthcare professionals who want to progress their career. However, it can feel like a daunting process on top of the demands of the day job and home life. This first part of our writing for publication series, provides guidance on what you need to do before you even begin to write.

In this article, three members of The Royal Marsden Pressure Ulcer Multidisciplinary Collaborative Group co-publish their personal reflections on the process of co-producing a new bedside document to prevent pressure ulcers.

It's fair to say that 2018 has been the year of the leg. Lower limb conditions are mainly managed using compression therapy as part of an evidence based approach to care. However, it seems that there is a gap between theory and practice. Here we ask specialists are some clinicians fearful of applying compression?

Brighton and Hove Clinical Commissioning Group (CCG), which serves a patient population of approximately 285,000, identified a number of problems around the prescribing and supply of wound dressings to the community. The use of an online non-prescription ordering service (ONPOS) by Coloplast was therefore implemented to drive efficiency and cost savings.

The National Wound Care Strategy Programme (NWCSP) has been developed to address the use of sub-optimal wound care. Here Una Adderley outlines how the NWCSP works, progress to date and how you can become involved as a stakeholder.

Most leg ulcers seen in practice are venous in aetiology. However, there are several atypical causes that you may come across from time to time. These should be considered if a leg ulcer is failing to heal as expected, despite best practice. Here atypical leg ulcer presentations are detailed.

A recently published paper in the journal Bioethical Inquiry by Sharp et al (2019) posed the provocative question in its headline ‘Two hourly repositioning for prevention of pressure ulcers in the elderly. Patient safety or elder abuse?’ Here some of you have your say.

Patient-clinician dialogue is important when delivering care to patients with chronic wounds. Here, a patient’s feelings relating to her management are detailed, and how the clinicians involved worked with her to accommodate them into her care.
Woundcare training is accessible to most healthcare professionals, but putting what is learnt into practice remains a challenge. This article presents some creative and practical approaches to helping staff translate what they have learnt into practice.