Resources
13 March 2023
About 20 women a day are diagnosed with ovarian cancer in the UK; that is approximately 7000 cases per year.1 The surface of the ovaries, fallopian tube and peritoneum are all close together making it difficult to distinguish where the cancer has started. Cancers that start in the ovary, fallopian tube or peritoneum often cause the same symptoms, are diagnosed using the same tests and are treated in the same way. The main treatments for these types of cancers are surgery and chemotherapy.1
01 March 2023
A specialist wound telehealth service was established to deliver equitable service with parity of access to wound care for all residents of 38 nursing homes in Sussex with wounds of any type (n=579). All patients were managed using a systematic telehealth approach that combined digital and in-patient consultations according to established protocols and care pathways. Data for a three-year period was analysed by hand to determine patient demographics, wound type and discharge outcomes for all patients with wounds. The results showed that the mean age of patients was 86 years, with the majority being female (80% healed and 66% deceased). Referral outcomes were referred onwards (n=92), healed (n=234) or deceased (n=253). The most prevalent wound type was pressure ulceration in both healed and deceased patient groups (60% and 59%, respectively), followed by lower limb wounds (20% and 26%, respectively). Mean time to healing or death were 103 days versus 86 days, respectively. The authors concluded that the collaborative use of a specialist wound telehealth service ensured that all residents received prompt, evidence-based wound care. Healing was achieved in this vulnerable patient population, despite the existence of numerous barriers to healing. Patients nearing end of life with a wound received palliative wound management. The time to healing in this group cannot be commented upon due to lack of comparative studies in this patient population.
28 February 2023
As healthcare professionals, our purpose is to deliver treatments and interventions to patients to aid recovery and prevent deterioration in health. But what does that look like when patients do not wish to follow advice, do not want treatment or interventions, even if that means significant consequences such as loss of limbs, sepsis or death — where do we legally stand in these situations and how do we work with patients to achieve the best possible outcomes for them? Over years of clinical experience, the authors have found that working with those who self-neglect can be complex. This is due to a range of factors, such as risks to the individual and sometimes others. Other issues involved include healthcare professionals’ views and moral conflict between respecting patient autonomy and their duty of care, challenges in trying to engage patients who may not want services involved, attempting to assess and being clear on the patient’s mental capacity, working within task-orientated systems which may not always be conducive to building rapport, and working with the patient’s socio-economic factors which impact upon their health (Research in Practice, 2020).
28 February 2023
When patients present with red lower legs, the cause is often assumed to be cellulitis or erysipelas. There are, however, several alternative conditions which mimic the clinical signs of cellulitis or erysipelas, which can lead to misdiagnosis. It is important that the cause is correctly diagnosed to prevent inappropriate prescribing of antibiotics.
28 February 2023
Dermatological conditions are notoriously difficult to spell! Psoriasis with its silent ‘P’ and eczema without an ‘X’. But how about hidradenitis suppurativa (HS)? Hard to spell, hard to pronounce but, more importantly, really hard to be a patient with the condition.
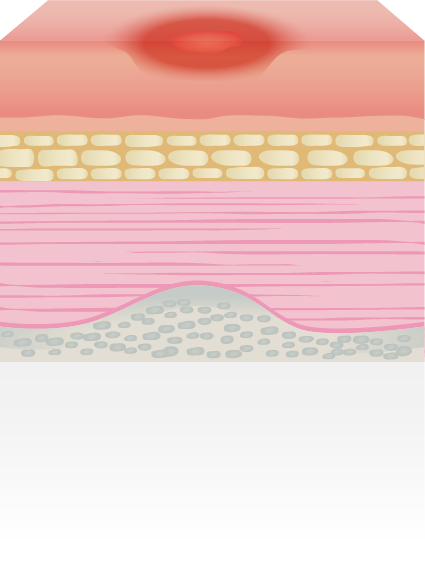
HS is a disease in which a patient develops boils and abscesses in the most intimate of areas (Figure 1); predominantly the groin and axillae.
HS is a disease in which a patient develops boils and abscesses in the most intimate of areas (Figure 1); predominantly the groin and axillae.
28 February 2023
Suboptimal management of leg ulcers has been identified as a UK-wide problem that is both costly to the NHS and a drain on nursing resources (Guest et al, 2020). The overall annual NHS cost of wound care has increased by 48% in real terms over the five years since Guest et al’s (2015) original work. Guest et al’s studies (2015; 2020) also found a common pattern with regard to a failure on the part of healthcare professionals to establish the underlying aetiology of a wound. This article highlights the importance of changing the way we treat leg ulceration in relation to identifying and managing patients with lymphovenous disease, and explores new treatments surrounding the care of leg ulceration to help break down fibrosis in complex wounds caused by lymphatic changes.
28 February 2023
This article explores why we should adapt assessment of leg ulceration to be more mindful of the presence of lymphoedema. If clinicians can change the assessment process and begin to treat leg ucleration with a lymphatic component differently to venous oedema, this, in turn, can potentially reduce complications such as toe, foot and knee oedema. The introduction of simple changes in documentation and additional training can lead to improved outcomes for patients as well as potential cost savings for healthcare providers.
06 September 2022
The delivery of wound care in the current climate is challenging so effective solutions are more important than ever. It is vital to be aware of the latest products and innovations that have the potential to improve outcomes.
Here, we present Mepitel® One, a gentle one-sided wound contact layer with Safetac® technology to minimise pain for patients during dressing changes.
Here, we present Mepitel® One, a gentle one-sided wound contact layer with Safetac® technology to minimise pain for patients during dressing changes.
29 October 2021
Monika Varechova describes her experience of using medical grade honey to achieve healing of bilateral chronic VLUs in a complex patient receiving palliative care.
26 October 2021
Karen Harrison Dening, Lisa Ashworth, Annemarie Brown, Teresa Burdett and Anne Williams discuss the different ways that nurses learn and how new technologies can help to engage all learners.










.jpeg)
 Success!
Success!